‘Getting to Zero’: PCDC in Mississippi


 Earlier this month, PCDC’s Mazdak Mazarei and Brandon Harrison drove 500 miles over three days in Mississippi. Their purpose: beginning new partnerships that will help improve HIV prevention services in the region.
Earlier this month, PCDC’s Mazdak Mazarei and Brandon Harrison drove 500 miles over three days in Mississippi. Their purpose: beginning new partnerships that will help improve HIV prevention services in the region.
Across visits to five federally qualified health centers (FQHCs), Mazarei and Harrison — both part of PCDC’s High Impact Prevention (HIP) in Health Care team — met staff and learned more about the local dynamics that will shape their work.
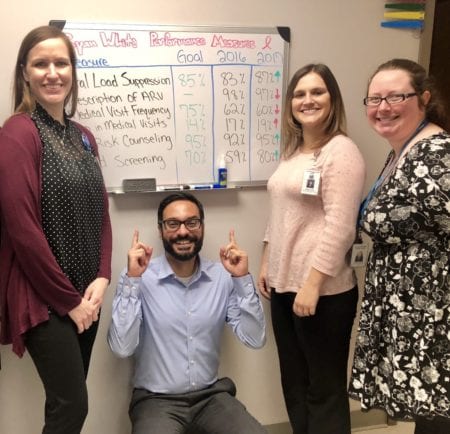
Mazarei [pictured], a senior project manager based in PCDC’s California office, talks below about key observations.
The five FQHCs are participating in what we’re calling “Getting to Zero” Learning Collaborative, a six-month initiative to help bring HIV transmissions to zero in Mississippi.
The collaborative will support the “Getting to Zero” vision of UNAIDS: zero new HIV infections, zero HIV deaths, and zero HIV stigma by 2020.
We worked with each of the organizations in advance to collectively identify areas of strength and improvement in their HIV prevention efforts.
We then visited them to build relationships, prioritize the work of our collaborative, link the organizations to tailored resources and capacity building assistance services, and devise next steps.
All of PCDC’s services — individualized coaching and guidance, monthly videoconferencing sessions, in-person learning sessions — will be provided at no cost.
This collaborative is also working in partnership with the Mississippi Primary Health Care Association and the Mississippi AIDS Education Training Center, who have longstanding capacity-building relationships with these health centers.
Studies and research show that HIV is prevalent in Mississippi — there are many more new diagnoses in the state, more so than in other parts of the country.
But at each of these five health centers — ranging from centers that are just starting to this work to places that are already Ryan White HIV/AIDS medical providers — very few had identified people living with HIV through testing within their health centers.
They didn’t necessarily know where these patients were, because they’re not identifying them through their own testing.
 In addition, as part of the HRSA funding they receive, FQHCs are tasked with asking all of their patients and clients about sexual orientation and gender identity. But there’s still so much stigma — to the extent that when we ask health centers how many patients they’ve seen in the past year who say they’re lesbian, gay, bisexual, transgender, or queer (LGBTQ), the answer is sometimes zero.
In addition, as part of the HRSA funding they receive, FQHCs are tasked with asking all of their patients and clients about sexual orientation and gender identity. But there’s still so much stigma — to the extent that when we ask health centers how many patients they’ve seen in the past year who say they’re lesbian, gay, bisexual, transgender, or queer (LGBTQ), the answer is sometimes zero.
And some of these centers have patient panels of over 1,000 people. So very few of their patients are self-identifying as LGBTQ.
That’s troubling for a couple of reasons. It means either people aren’t feeling safe in general to say they’re LGBTQ, or that people who are LGBTQ aren’t accessing services at these centers, which as safety-net providers provide very essential services.
Which begs the question, where are these people accessing services, if they’re accessing services at all? That’s definitely something we want to partner on addressing.
We visited Delta Health Center, the first FQHC anywhere in the U.S., founded by Dr. Jack Geiger [a recent PCDC champion]. They have what’s most important in integration work: strong champions within who support HIV integration work. Staff at all levels have the energy to say, “Yes, let’s do this.”

Mazarei [left] and Harrison with Delta Health Center’s Joyce Roundtree-McCoy, Grants Project Coordinator, and Robin Boyles, Director of Planning and Development.
It’s a credit to their leadership, and it’s the most critical element.
For example, take someone who might have been a patient as a child, and who gets diagnosed with HIV later in life. The health center doesn’t want to tell that person that they can’t receive care at the center anymore, or send them up to 100 miles away to the nearest facility providing HIV services.
The provider wants to continue to serve those people as part of its community, as part of its care.
That’s what Delta Health Center is working towards. And the center’s really excited to be expanding its capacity, to be able to do this work again in a way that’s sustainable.
The region is a draw for organizations in that there’s a lot of need, but we heard that “too many swoop out too quickly after swooping in.”
When we talk to local organizations that’ve worked successfully in a sustainable way, they always mention the importance of relationship-building. You need to go there in person and get to know people as people, to build that trust, so you’re not just a temporary presence who’s there just to meet your numbers.
It was really important for us to plant the seed for building what will hopefully be long-term relationships with these centers.
Something great about being part of PCDC is that it’s not only us — the Capacity Building team — who will work with these organizations. It’s also a priority of PCDC’s Community Investment team to invest actual dollars to help build infrastructure. It’s nice to be able to provide both of those services in a complementary way.
It really demonstrates a comprehensive investment in these communities. And it’s important for several reasons.
We’re putting financing, resources, and efforts where our mouths are.
We’re putting in the time to work with organizations to identify their own needs instead of telling them what to do.
We’re taking the time to listen and create the space for folks to come up with solutions themselves.
And we’re providing resources and connecting local organizations to resources — because they’re the ones who know their populations best.