Data-Driven Operations & Change
PCDC supports organizations to leverage data to drive improvements in their operations, access, and impact.
PCDC supports organizations to leverage data to drive improvements in their operations, access, and impact.
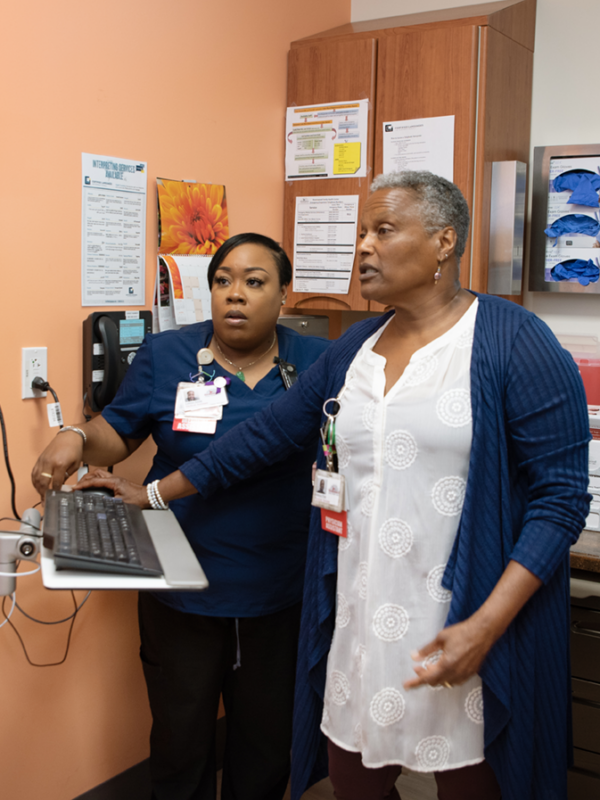
Our staff guide health care providers through change and improvement – whether focused on screening or testing, access to appointments, or performance on quality measures. Our coaches support organizations to leverage their existing data and strengths to achieve improvements in processes, outcomes, and, ultimately, health equity.
Providers face increasing complexity to meet their communities’ health care needs, including changing regulations, incentives, and payment models, and an increasing focus on behavioral health and social drivers of health. Primary care providers are becoming increasingly aware of the impact of social drivers on health, as well as persistent disparities in access and outcomes among historically marginalized communities.
We use evidence-based quality improvement strategies to support practices through change, leveraging the assets and strengths that are already present within the organization and the community. Our solutions are practical and actionable and help organizations take ownership of their practice’s strategic goals.
Our staff are experts in addressing common practice challenges through evidence-based quality improvement, including: